The Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) requires employers to offer covered employees who lose their health benefits due to a qualifying event to continue group health benefits for a limited time at the employee’s own cost.
What is a COBRA Qualifying Event?
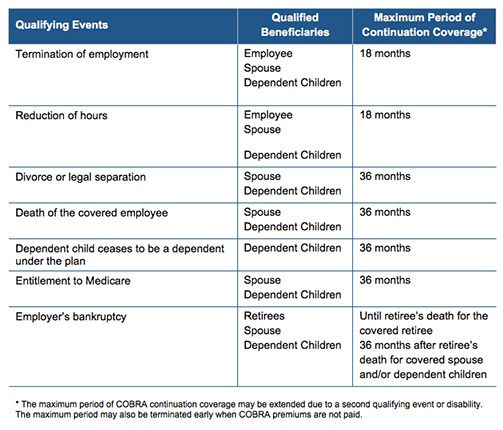
Per regulation, COBRA qualifying events are specific events that cause or trigger an individual to lose health coverage. The type of qualifying event determines who the qualified beneficiaries are and the maximum length of time a plan must offer continuation coverage. A group health plan may provide longer periods of continuation coverage beyond the maximum 18 or 36 months required by law.
There are seven triggering events that are qualifying events for COBRA coverage if they result in loss of coverage for the qualified beneficiaries, which may include the covered employee, the employee’s spouse, and dependent children.
The following quick reference chart indicates the qualifying event, the individual who is entitled to elect COBRA, and the maximum length of COBRA continuation coverage.
By Danielle Capilla
Originally Published By United Benefit Advisors
We're here to help.
Schedule a free phone consultation today.
Latest Insights
Advanced Estate & Insurance Services, Inc. CA License #0M90887
Duda Website Design & SEO by RivalMind